The Most Notable Medical Findings of 2016
“At
least you have your research world, where there are facts,” a
journalist friend told me recently. He was referring, of course, to the
sharp Orwellian turn that our public discourse has taken in the past
year, when practically anyone who traffics in truth—scientists,
reporters, intelligence experts, cyber-security specialists—has been
dismissed by our President-elect as a liar or a shill. My friend was
right: research has indeed provided a respite from the maddening media
conversation, a chance to challenge the assumptions and biases of
medical science and public health not with bluster and noise but with
rigorous experimentation. It was with this in mind that I selected the
notable findings of 2016. Welcome to the sanctuary.
Exculpating Patient Zero
The
history of medicine, like the history of the justice system, is filled
with cases of wrongful conviction. In the Middle Ages, for instance,
Jews were accused of having orchestrated an outbreak of the Black Death
by poisoning town wells; there were pogroms across Europe. In our era,
the epidemic was AIDS and the scapegoat was Gaëtan Dugas,
a gay flight attendant from Quebec. He featured prominently in “And the
Band Played On,” Randy Shilts’s best-selling book from 1987, in which
Dugas was identified as Patient Zero—that is, the person responsible for
bringing the disease to the continental United States. Shilts’s
characterization of Dugas as a “suave Quebecois” who travelled the world
having high-risk sex was seized upon by homophobes as proof that the
wages of sin is death. As a result, the Reagan Administration was
shamefully passive in the face of an explosive epidemic, and some
medical researchers, similarly colored by prejudice, initially dubbed
the disease GRID, for “gay-related immune deficiency,”
despite evidence of infection among straight immigrants from the
Caribbean and hemophiliacs who had received transfusions of tainted
blood.
 Dugas succumbed to an AIDS-related cancer in 1984, but a sample of the H.I.V. strain that he carried was preserved. Earlier this year, in the journal Nature, the evolutionary biologist Michael Worobey and his colleagues reported that they had performed a genetic analysis of the sample,
along with others from early on in the epidemic. Dugas, they concluded,
was not Patient Zero, not the first carrier of H.I.V. to America;
rather, their analysis revealed that the virus arrived in New York City
from the Caribbean in the nineteen-seventies, a decade before Dugas
entered our country. They trace the mistake to a simple typo: as
investigators from the Centers for Disease Control and Prevention were
attempting to track the AIDS outbreak, they labelled
Dugas Patient O, where “O” indicated that he resided “outside of
California.” Finally, science has corrected the record. This serves as a
cautionary tale for medical professionals, journalists, and laypeople
alike to resist clinical indictments based on hearsay, if not outright
imagination.
Dugas succumbed to an AIDS-related cancer in 1984, but a sample of the H.I.V. strain that he carried was preserved. Earlier this year, in the journal Nature, the evolutionary biologist Michael Worobey and his colleagues reported that they had performed a genetic analysis of the sample,
along with others from early on in the epidemic. Dugas, they concluded,
was not Patient Zero, not the first carrier of H.I.V. to America;
rather, their analysis revealed that the virus arrived in New York City
from the Caribbean in the nineteen-seventies, a decade before Dugas
entered our country. They trace the mistake to a simple typo: as
investigators from the Centers for Disease Control and Prevention were
attempting to track the AIDS outbreak, they labelled
Dugas Patient O, where “O” indicated that he resided “outside of
California.” Finally, science has corrected the record. This serves as a
cautionary tale for medical professionals, journalists, and laypeople
alike to resist clinical indictments based on hearsay, if not outright
imagination.Your Bubbe Is Not Always Right
Everyone
loves a folk remedy. For more than a century, grandmothers and
physicians have prescribed cranberry juice as a cure for urinary-tract
infections, which are caused by bacteria in the bladder and urethra.
Like many tenacious folk remedies, this one appears to have some basis
in science. Quinic acid, which is present in cranberries, is metabolized
by the body into hippuric acid, a substance that in very high
concentrations is toxic to E. coli, the pathogen most commonly
to blame for U.T.I.s. Researchers have also found that lectins,
carbohydrate-rich molecules in cranberries, can (in a test tube, at
least) prevent E. coli from attaching to the cells that line the urinary tract.
Alas, the wisdom of the bubbe often collapses under rigorous testing. Last month, researchers at the Yale School of Medicine published the results of
an investigation into the cranberry remedy. They performed their study
in nursing homes, where U.T.I.s are common, giving a hundred and
eighty-five women aged sixty-five and older either cranberry capsules or
a placebo. (Neither the participants nor the researchers knew what was
given to whom.) The result was striking: the two groups showed no
difference in either the number of symptomatic infections or the
presence of bacteria in the urine. Furthermore, the group given
cranberry capsules required as much antibiotic treatment as the placebo
group to eradicate the bugs.
While
other experiments have suggested the same results before, they were
conducted with small numbers of patients. The Yale study is more
definitive. Still, I am skeptical that the cranberry market will collapse.
Folk wisdom has a way of overcoming science, as Gwyneth Paltrow and
Michael Phelps have proved with their obsession over cupping, an ancient
therapy lately given new life. On the other hand, maybe bubbes aren’t
always wrong. As they say in Yiddish, “Es vet helfn vi a toytn bankes”—“It’s as helpful as cupping a corpse.”
Rethinking Prostate Cancer
For
many years, American physicians have screened their older male patients
for prostate cancer by looking at the level of a particular protein in
the blood. The protein, called prostate-specific antigen (P.S.A.), can
indicate the presence of a tumor long before any symptoms materialize.
Recently, though, there has been a movement within the medical community
against P.S.A. testing; since prostate cancers typically grow very
slowly and rarely cause discomfort, the thinking goes, early screening
may not be all that useful. The U.S. Preventive Services Task Force,
based on data from two large clinical trials, currently recommends
against routine screening, but other expert groups (using the same
evidence) have countered that men should be allowed to choose for
themselves.
Now the dispute has become even more fraught. In October, The New England Journal of Medicine published a study by
a group of British researchers that examined three classes of
prostate-cancer patients: those who had received surgery, those who had
received radiation therapy, and those whose disease had been carefully
monitored without intervention. After ten years, there was no difference
in survival rates among the three groups. Active treatment does not
change the over-all risk of death, and this was the headline in most
news reports. But largely overlooked in the press was that metastases,
meaning spread of the cancer beyond the prostate gland to tissues in the
pelvis and to bone, occurred three times more frequently in those being
monitored than in those who received surgery or radiation. Not
surprisingly, the cancer also progressed more quickly in these men.
In an editorial that
accompanied the study, Anthony D’Amico, a radiation oncologist at
Boston’s Dana-Farber Cancer Institute, argued that men should be
informed of the risk of metastasis and of its consequences, particularly
pelvic tumors and bone pain and fracture. D’Amico advises that men who
wish to avoid metastases should consider monitoring, rather than surgery
or radiation, only if their life expectancy is less than a decade.
Having cared for many men with prostate cancer that metastasized—an
incurable situation often marked by severe suffering—I strongly concur.
A Knife in the Back, Again
As
we age, the wear and tear on our joints can not only erode cartilage
but also cause bone to overgrow. Bone spurs are familiar in the feet and
knees, but they can occur in the spine as well, narrowing both the
central canal through which nerves pass and the small openings, called
foramina, where they exit. This narrowing is termed spinal stenosis, and
has characteristic symptoms: walking exacerbates the condition, causing
pain and muscle weakness, and rest makes it subside. Physical therapy
and anti-inflammatory agents can afford some relief, but many patients
ultimately require surgery, particularly if there is a chance that
muscle strength will be permanently lost.
Spinal
surgery is lucrative. A simple laminectomy, in which the back portions
of a couple vertebrae are removed in order to widen the canal, might
cost five or seven thousand dollars. But a popular addition to
laminectomy is a so-called fusion, in which adjoining vertebrae are
connected with titanium hardware, keeping them aligned and the spine
stable. This raises the price to fifteen thousand or twenty thousand
dollars, or more. Perhaps as a result, there has been a sharp rise in
the number of fusion surgeries in the United States: between 2002 and
2007 alone, the increase was fifteen-fold.
Fortunately, we now have data that may temper the drive for fusion surgery. In April, Swedish scientists published the results of
an inquiry into spinal-stenosis treatments, examining nearly two
hundred and fifty patients who had been randomly assigned to undergo
laminectomy alone or added fusion. After two years, both groups of
patients functioned equally well. Those who had received fusions, of
course, had spent more time in the hospital, experienced more
complications, and cost the Swedish health-care system a good deal more
money.
I have never suffered from
spinal stenosis, but more than a decade ago I underwent fusion surgery
for back pain and “concern” over spinal instability. As I noted in an
essay for the magazine called “A Knife in the Back,”
the procedure left me in more pain than before and limited my
functioning for years. In spine surgery, it seems, less may not be more,
but it can be equivalent.
Under the Gun
We
usually think of public-health measures as targeting the pathogens and
substances that cause our bodies harm—viruses, tainted drinking water,
addictive drugs like oxycodone and heroin. But one of the leading
threats to the health of the nation is access to firearms. For the past
twenty years, the C.D.C. has largely refrained from investigating gun
deaths as a public-health issue; although the agency tracks them, it was
forbidden by Congress, in 1996, from spending money to “advocate or
promote gun control,” and the effects of that measure have lingered.
(“I’m sorry, but a gun is not a disease,” the former House Speaker John
Boehner said last year.)
Fortunately, Australians seem to have no such delusions. In July, researchers at the University of Sydney published an analysis of
how a major reform law from 1996, which banned semiautomatic rifles and
pump-action shotguns and created an extensive gun-buyback program, has
affected firearm fatalities in the country. In the seventeen years
before the law was passed, thirteen mass shootings occurred in
Australia; since 1996, there have been none. In addition, the authors
note, there was a two-thirds decline in the over-all rate of firearm
deaths.
Beyond these compelling
numbers, there are lessons to be learned in the political arena. The
Australian legislation was a direct reaction to a mass shooting in Port
Arthur, Tasmania, in which thirty-five people were murdered and at least
eighteen were wounded by an assailant with a semiautomatic rifle. The
public outcry brought together Australia’s political parties from the
right and left; indeed, it was a conservative Prime Minister, John
Howard, who spearheaded the reform. Shamefully, nothing of the sort
followed the killing of twenty children and six adults in Newtown,
Connecticut, in 2012, or the attack on the Orlando, Florida, night club
this June that resulted in the deaths of forty-nine victims. The recent
data from Australia should remind us that our politicians’ failure to
keep high-powered weapons out of public circulation is utterly
inexcusable.
Jerome Groopman, a staff writer since 1998, writes primarily about medicine and biology.




 En 1516, c'est au tour des Ottomans de s'y implanter. Sous leur tutelle, Vénitiens, Français et Anglais s'invitent dans ce lieu commercial stratégique. Ces nations finissent par s'en désintéresser au profit de leurs colonies, marquant ainsi le déclin de la ville de nouveau fragilisée par un important séisme en 1822.
En 1516, c'est au tour des Ottomans de s'y implanter. Sous leur tutelle, Vénitiens, Français et Anglais s'invitent dans ce lieu commercial stratégique. Ces nations finissent par s'en désintéresser au profit de leurs colonies, marquant ainsi le déclin de la ville de nouveau fragilisée par un important séisme en 1822.
 Au cœur de la ville se dresse l'ancien tell de la cité néo-hittite (Xe s. av. J.-C.).
Au cœur de la ville se dresse l'ancien tell de la cité néo-hittite (Xe s. av. J.-C.).

 Depuis le XIIe siècle, sur plus de 10 kilomètres d'allées en contrebas de la citadelle, les petites boutiques du vieux marché s'alignent suivant leur spécialité dans un désordre très organisé.
Depuis le XIIe siècle, sur plus de 10 kilomètres d'allées en contrebas de la citadelle, les petites boutiques du vieux marché s'alignent suivant leur spécialité dans un désordre très organisé. Au IX s., les Qarmates, membres d'une secte chiite, organisèrent ces ensembles en veillant à la qualité des produits et créant des taxes.
Au IX s., les Qarmates, membres d'une secte chiite, organisèrent ces ensembles en veillant à la qualité des produits et créant des taxes.



 Toujours en activité, les savonneries font la réputation d'Alep depuis l'époque ayyoubide, au XIIe s. À la veille de la guerre civile, elles produisaient encore 25 000 pièces par jour (6 tonnes).
Toujours en activité, les savonneries font la réputation d'Alep depuis l'époque ayyoubide, au XIIe s. À la veille de la guerre civile, elles produisaient encore 25 000 pièces par jour (6 tonnes). Bâtiment moderne sans charme, le musée archéologique d'Alep a pourtant une importance considérable : il renferme les trésors archéologiques de la région, en particulier des villes de Mari (XXXe s. av. J.-C.), d'Ebla (XXIV s. av. J.-C.) et d'Ougarit (XIIIe s. av. J.-C.) qui sont aux sources de la civilisation.
Bâtiment moderne sans charme, le musée archéologique d'Alep a pourtant une importance considérable : il renferme les trésors archéologiques de la région, en particulier des villes de Mari (XXXe s. av. J.-C.), d'Ebla (XXIV s. av. J.-C.) et d'Ougarit (XIIIe s. av. J.-C.) qui sont aux sources de la civilisation.










 Celui-ci,
confronté à la menace des redoutables Lombards, ne peut plus compter
sur la protection de l'empereur de Constantinople, lequel a d'autres
soucis avec les Bulgares et les Arabes. L’empereur a, qui plus est,
décidé d’interdire les images religieuses. Or, le pape condamne
formellement l’
Celui-ci,
confronté à la menace des redoutables Lombards, ne peut plus compter
sur la protection de l'empereur de Constantinople, lequel a d'autres
soucis avec les Bulgares et les Arabes. L’empereur a, qui plus est,
décidé d’interdire les images religieuses. Or, le pape condamne
formellement l’



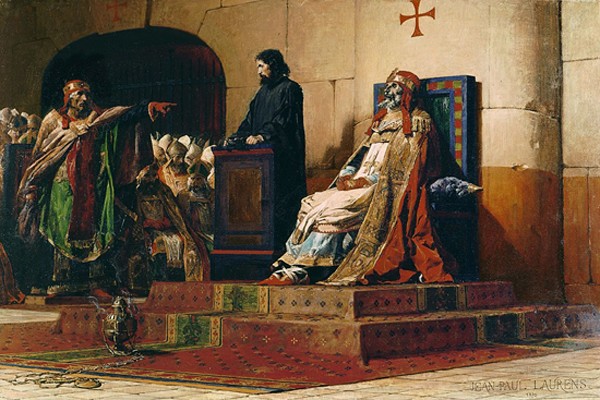
 Serge III (904-911) fait la fortune du clan de Tusculum, représenté par le comte Théopylacte et son épouse Théodora. Ses opposants l'accusent d’être l’amant de leur fille Marousie.
Serge III (904-911) fait la fortune du clan de Tusculum, représenté par le comte Théopylacte et son épouse Théodora. Ses opposants l'accusent d’être l’amant de leur fille Marousie.

 Il
impose sur le trône de saint Pierre son précepteur Gerbert d’Aurillac,
qui devient pape sous le nom de Sylvestre II (999-1003). Tout un
programme.
Il
impose sur le trône de saint Pierre son précepteur Gerbert d’Aurillac,
qui devient pape sous le nom de Sylvestre II (999-1003). Tout un
programme. Thomas Tanase, diplômé de l’Institut d’Études politiques de Paris, est docteur et professeur agrégé d’histoire.
Thomas Tanase, diplômé de l’Institut d’Études politiques de Paris, est docteur et professeur agrégé d’histoire.


 Il
soumet les populations côtières, apparentées quant à elles aux
Mélanésiens, notamment les Sakalavas de la côte occidentale (autour du
port de Majunga), les Betsileo des plateaux méridionaux (autour de
Fianarantsoa) et les Betsimisarakas de la côte orientale (autour du
grand port de Tamatave).
Il
soumet les populations côtières, apparentées quant à elles aux
Mélanésiens, notamment les Sakalavas de la côte occidentale (autour du
port de Majunga), les Betsileo des plateaux méridionaux (autour de
Fianarantsoa) et les Betsimisarakas de la côte orientale (autour du
grand port de Tamatave).
 Radama
1er, fils et successeur du grand roi, achève la soumission de l'île
avec l'appui du gouverneur britannique de l'île Maurice voisine et de
nombreux experts européens.
Radama
1er, fils et successeur du grand roi, achève la soumission de l'île
avec l'appui du gouverneur britannique de l'île Maurice voisine et de
nombreux experts européens. Radama
II, fils et successeur de la reine en 1861, rouvre les ports aux
Européens. Mais il est rapidement assassiné et sa veuve, Rasoherina,
épouse son Premier ministre, Rainilairivony, lequel va s'attribuer la
réalité du pouvoir en se remariant avec les reines suivantes, Ranavalo
II et Ranavalo III.
Radama
II, fils et successeur de la reine en 1861, rouvre les ports aux
Européens. Mais il est rapidement assassiné et sa veuve, Rasoherina,
épouse son Premier ministre, Rainilairivony, lequel va s'attribuer la
réalité du pouvoir en se remariant avec les reines suivantes, Ranavalo
II et Ranavalo III.

 Philibert
Tsiranana, ancien instituteur à l'accent languedocien inimitable (il a
fait ses études à Montpellier) en devient le premier président de la
République.
Philibert
Tsiranana, ancien instituteur à l'accent languedocien inimitable (il a
fait ses études à Montpellier) en devient le premier président de la
République. Marc
Ravalomanana, un jeune chef d'entreprise élu démocratiquement à la
présidence de la République, suscite un immense espoir dans le pays.
Marc
Ravalomanana, un jeune chef d'entreprise élu démocratiquement à la
présidence de la République, suscite un immense espoir dans le pays.